Antibiotics are among the most significant medical discoveries in human history. They have saved countless lives by treating bacterial infections that were once fatal. However, while antibiotics are highly effective at eliminating harmful bacteria, they also come with a lesser-known side effect — they can disrupt the delicate ecosystem of microorganisms living in your gut. This community, known as the gut flora or microbiota, plays a vital role in digestion, immunity, and even mental health.
Understanding how antibiotics change your gut flora and learning how to support digestive health recovery afterward is essential for maintaining long-term wellness. Let’s explore how antibiotics work, what happens to your gut microbiome during treatment, and the best strategies to restore balance using diet, lifestyle, and probiotics.
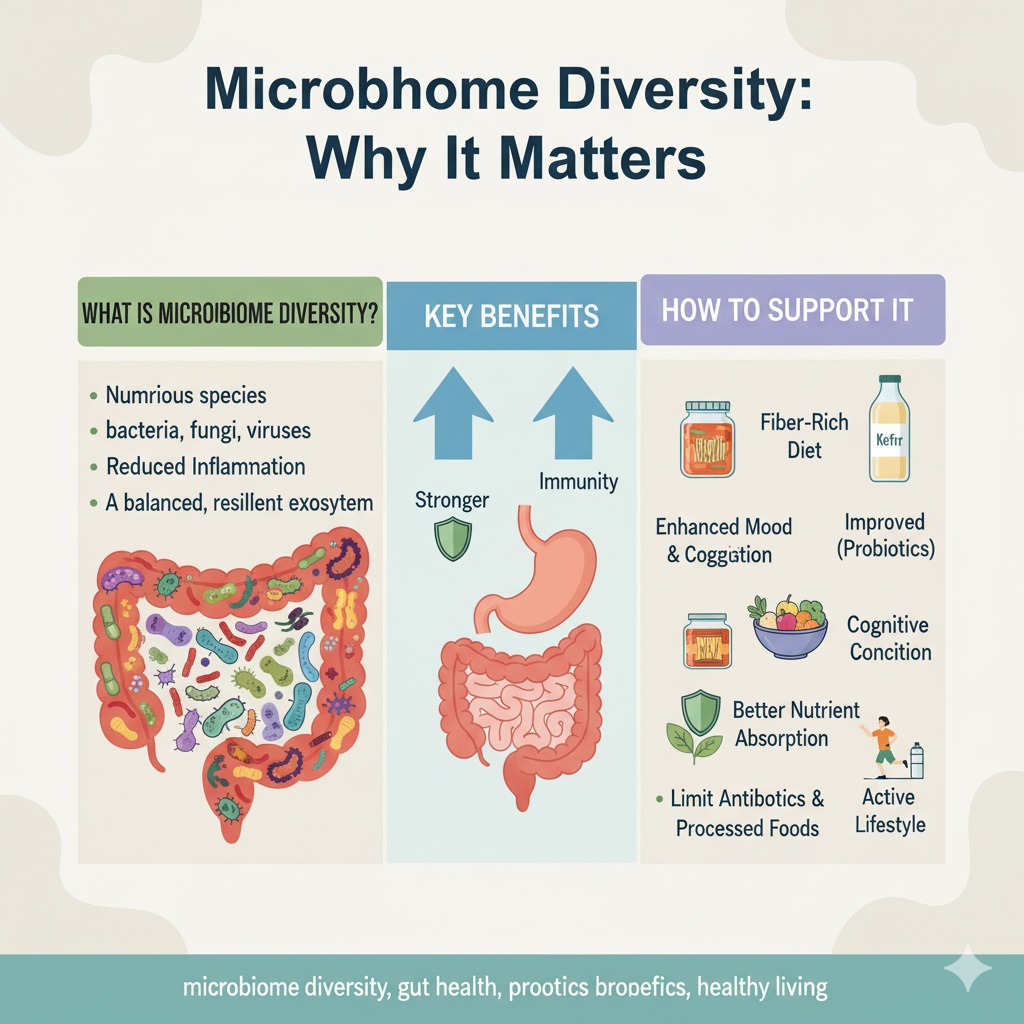
What Is Gut Flora and Why Does It Matter?
Your gut flora consists of trillions of microorganisms — bacteria, fungi, viruses, and yeasts — that reside primarily in the large intestine. These microbes help break down complex carbohydrates, produce essential vitamins like B12 and K, and regulate the immune system.
In a balanced state, your gut microbiome supports digestion, prevents infection, and helps maintain the intestinal barrier. However, when this balance is disturbed, it can lead to digestive discomfort, inflammation, and even more serious health concerns such as irritable bowel syndrome (IBS), obesity, and mood disorders.
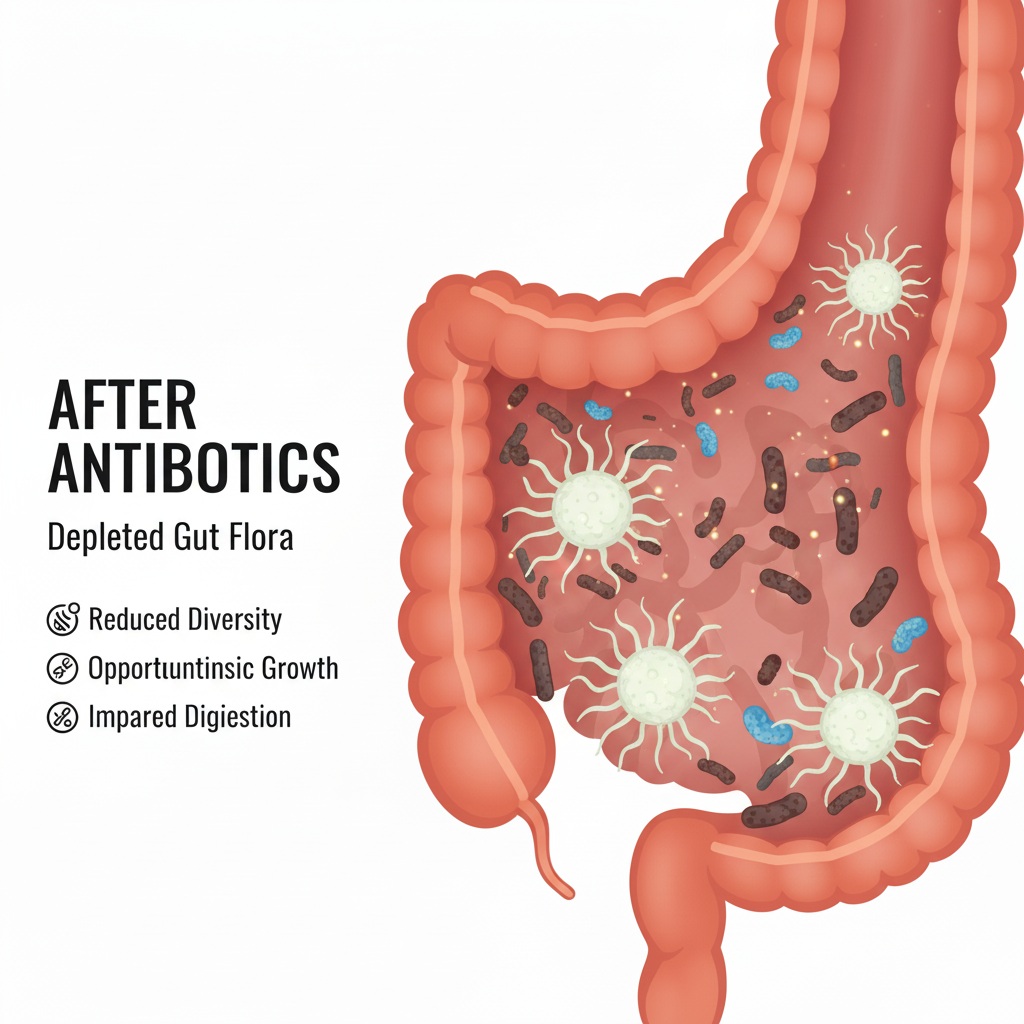
How Antibiotics Affect Gut Flora
Antibiotics work by targeting and killing bacteria. Unfortunately, they are not selective — they eliminate both harmful pathogens and beneficial bacteria. The extent of this disruption depends on several factors, including the type of antibiotic, dosage, and duration of use.
1. Reduction in Microbial Diversity
One of the most immediate effects of antibiotic use is a reduction in microbial diversity. A healthy gut contains a wide variety of bacterial species that maintain balance and resilience. After antibiotic treatment, this diversity can drop dramatically, allowing opportunistic or harmful bacteria to dominate.
2. Overgrowth of Pathogenic Bacteria
With beneficial bacteria reduced, harmful species like Clostridium difficile or Candida albicans can thrive. These overgrowths can cause infections, diarrhea, and even more serious complications, especially in individuals with weakened immune systems.
3. Altered Metabolism and Nutrient Absorption
The gut microbiota is responsible for breaking down dietary fibers into short-chain fatty acids (SCFAs), which are crucial for colon health. Antibiotic-induced disruption can decrease SCFA production, affecting energy metabolism and nutrient absorption.
4. Impact on the Immune System
Because 70% of the immune system resides in the gut, any disturbance in gut flora directly impacts immune function. Antibiotics can weaken immune response and make the body more vulnerable to infections in the short term.
Can Gut Flora Recover After Antibiotics?
The good news is that the gut microbiome is remarkably resilient. For most people, it can recover within a few weeks to months after antibiotic treatment. However, full restoration depends on several factors — such as diet, age, and overall health.
In some cases, repeated or long-term antibiotic use can cause lasting changes in microbial composition. This is why proactive measures to support digestive health recovery are essential after taking antibiotics.
Steps to Support Digestive Health Recovery
Rebuilding a healthy gut after antibiotics requires a combination of dietary, lifestyle, and supplemental strategies. Below are scientifically supported ways to promote gut healing and restore balance.
1. Eat a Fiber-Rich Diet
Dietary fiber is the most powerful fuel for beneficial gut bacteria. High-fiber foods — such as oats, legumes, bananas, apples, and leafy greens — help feed probiotics and encourage bacterial diversity. Aim to consume 25–35 grams of fiber per day.
2. Include Fermented Foods
Fermented foods are natural sources of probiotics — live microorganisms that promote gut health. Adding yogurt, kefir, sauerkraut, kimchi, and kombucha to your diet can help repopulate beneficial bacteria and restore microbial balance.
3. Take Probiotic Supplements
Probiotics are among the most effective ways to restore gut flora after antibiotics. Research shows that strains such as Lactobacillus acidophilus, Bifidobacterium lactis, and Saccharomyces boulardii can shorten antibiotic-associated diarrhea and improve microbiota recovery.
For best results, take probiotics at least two hours after your antibiotic dose and continue for several weeks after finishing the course.
4. Don’t Forget Prebiotics
Prebiotics are non-digestible fibers that serve as food for probiotics. Examples include inulin (found in chicory root), fructooligosaccharides (FOS), and resistant starches from foods like cooked and cooled potatoes. Combining probiotics and prebiotics — known as synbiotics — enhances the growth of beneficial bacteria.
5. Stay Hydrated
Water supports healthy digestion and helps maintain the mucosal lining of the gut. It also assists in the elimination of toxins and bacterial by-products that can accumulate during antibiotic treatment.
6. Avoid Processed Foods and Added Sugars
Refined sugars and processed foods feed harmful bacteria and yeast, which can further disrupt gut balance. Reducing sugar and artificial additives helps create an environment where beneficial microbes can flourish again.
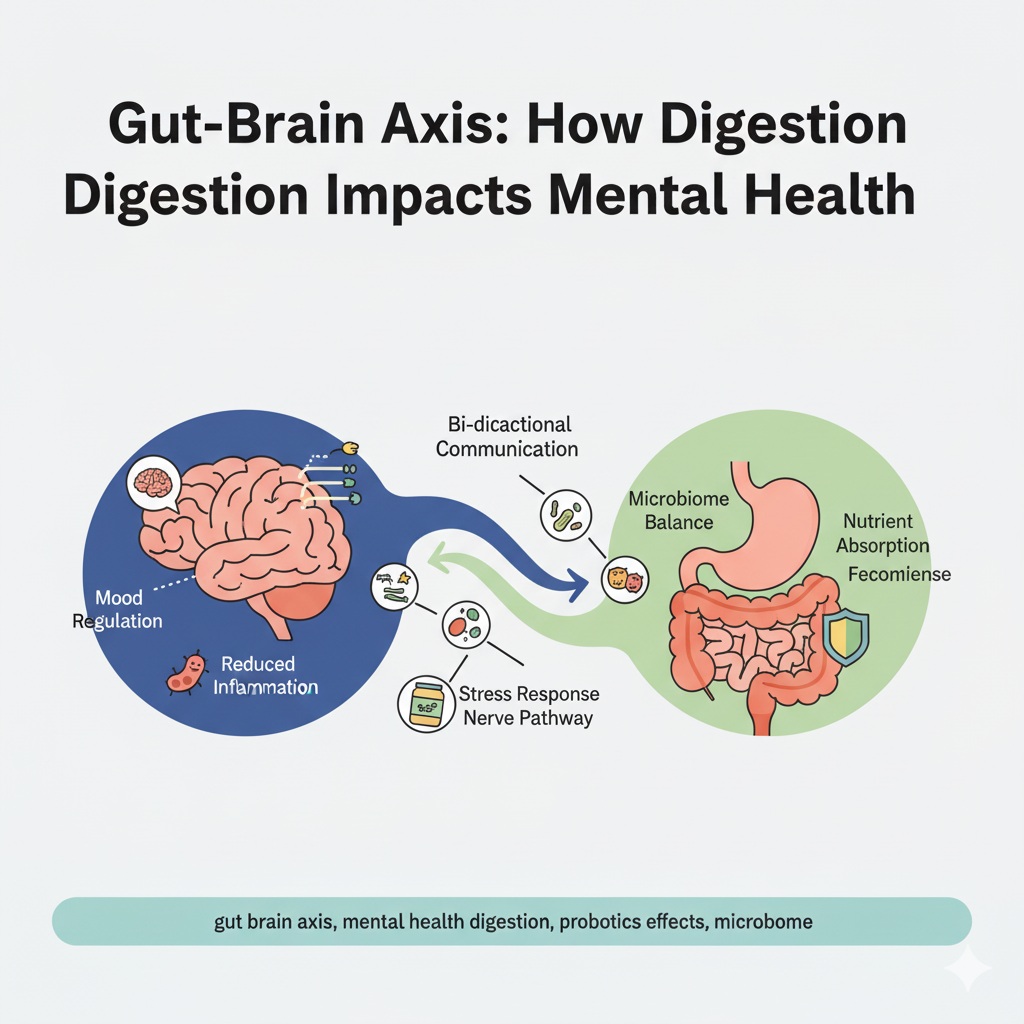
7. Get Enough Sleep and Manage Stress
Sleep deprivation and chronic stress negatively impact gut health through the gut-brain axis. Practices like meditation, yoga, and deep breathing can help lower cortisol levels and promote microbiome stability.
8. Limit Alcohol and Caffeine
While moderate alcohol and coffee consumption may not be harmful for everyone, excessive intake can irritate the intestinal lining and hinder bacterial recovery. It’s best to limit both during your healing period.
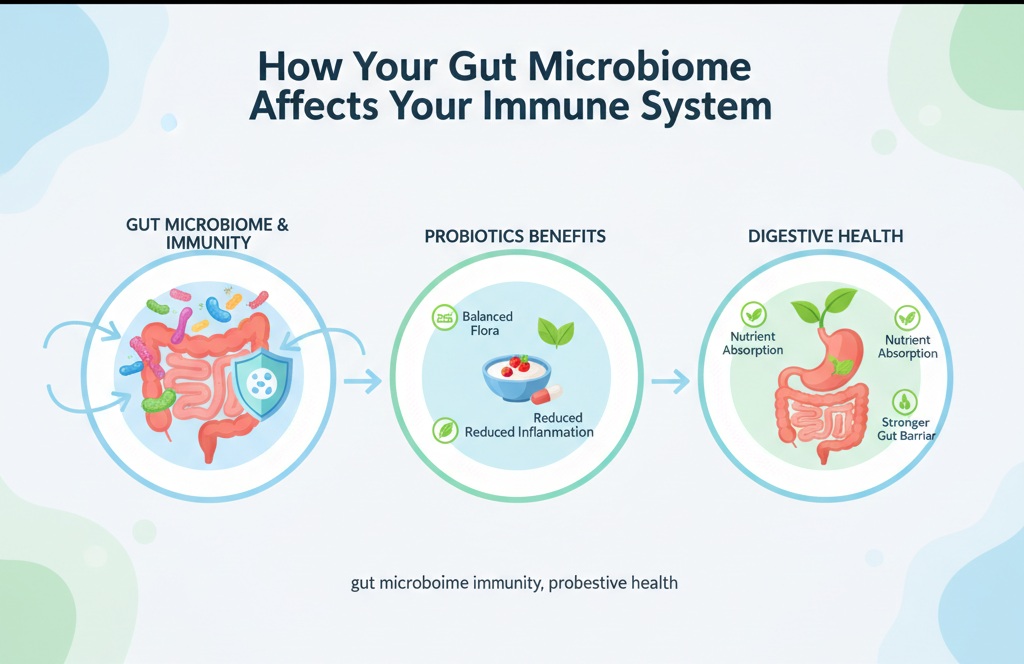
The Role of Probiotics in Gut Flora Restoration
Probiotics deserve special attention when it comes to antibiotic recovery. Clinical studies consistently show that taking probiotics can reduce the risk of antibiotic-associated diarrhea by up to 50%. Moreover, they help restore microbial diversity faster and improve immune response.
When choosing a probiotic supplement, consider the following:
- Look for multi-strain formulas containing at least 10 billion CFU per serving.
- Choose clinically tested strains like Lactobacillus rhamnosus GG or Bifidobacterium longum.
- Opt for delayed-release capsules, which protect probiotics from stomach acid.
Consistency is key — regular intake over several weeks provides the best results for digestive health recovery.
Long-Term Implications of Antibiotic Use
While short-term antibiotic use is generally safe, overuse can lead to long-term consequences. Chronic alterations in gut flora may increase susceptibility to metabolic and immune-related disorders such as obesity, type 2 diabetes, allergies, and inflammatory bowel disease.
Therefore, antibiotics should always be used responsibly — only when prescribed by a healthcare professional and for bacterial infections, not viral ones like the common cold or flu.
The Future of Gut Health Research
Modern science is increasingly exploring the connection between gut microbiota and overall well-being. Researchers are investigating ways to create targeted antibiotics that kill harmful bacteria without harming beneficial microbes. Additionally, advances in microbiome therapy, such as fecal microbiota transplantation (FMT), are showing promise in restoring gut balance in severe cases.
Personalized nutrition and microbiome testing are also emerging fields, allowing individuals to tailor diets and supplements according to their unique gut profiles.
Conclusion
Antibiotics are life-saving medicines, but they can also disrupt the complex ecosystem that keeps your digestive system healthy. Understanding how antibiotics change your gut flora — and taking steps to support recovery through probiotics, prebiotics, and balanced nutrition — is essential for long-term wellness.
By nurturing your gut after antibiotic use, you can restore microbial diversity, strengthen your immune system, and improve your overall health from the inside out.