Antibiotics are among the most important medical discoveries of the 20th century. They have saved countless lives by fighting bacterial infections that were once deadly. However, while antibiotics are powerful and effective, they can also have unintended side effects—particularly on your digestive system.
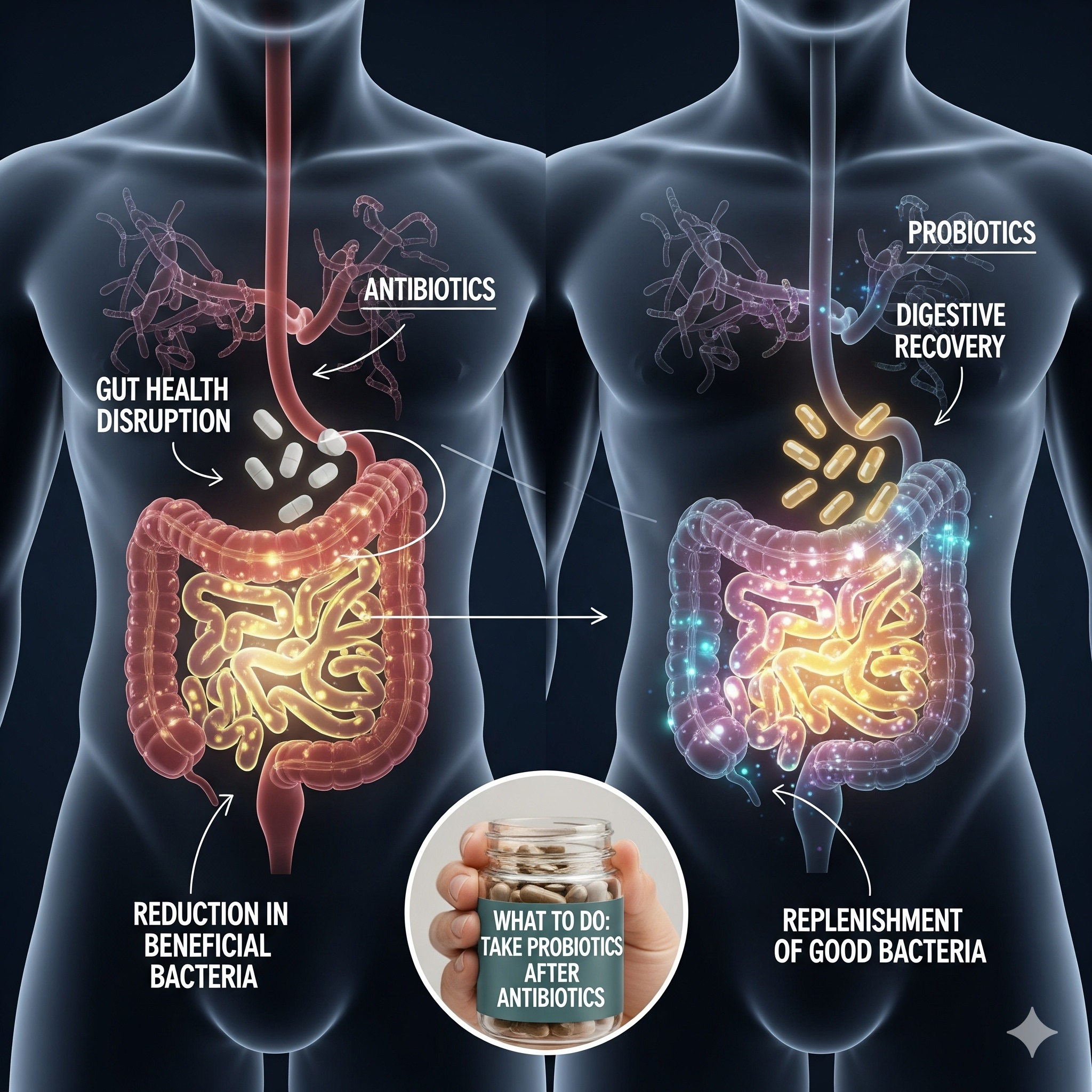
Your gut is home to trillions of bacteria that play a vital role in digestion, immunity, and overall wellness. Unfortunately, antibiotics don’t discriminate between harmful bacteria and the beneficial microbes that keep your gut healthy. This can lead to short-term discomfort and long-term imbalances if not managed properly.
In this article, we’ll explore how antibiotics affect gut health, the importance of probiotics after antibiotics, and practical steps you can take for digestive recovery.
Why Gut Health Matters
The gut is often referred to as the “second brain” because of its close connection to the nervous system and its major influence on overall health. The gut microbiome—made up of bacteria, fungi, and other microorganisms—contributes to:
- Breaking down food and absorbing nutrients
- Supporting the immune system
- Producing vitamins like B12 and K
- Balancing mood through neurotransmitter production
- Protecting against harmful pathogens
A healthy gut is key to maintaining energy, immunity, and mental clarity. When antibiotics disrupt this balance, the consequences can be felt throughout the body.
How Antibiotics Affect Your Gut
1. Reduction of Beneficial Bacteria
Antibiotics wipe out both good and bad bacteria. This loss of beneficial microbes reduces microbial diversity, which is essential for gut health.
2. Digestive Discomfort
Many people experience bloating, gas, cramping, diarrhea, or constipation during or after antibiotic treatment. These are signs that your digestive balance has been disturbed.
3. Overgrowth of Harmful Bacteria
When beneficial bacteria are suppressed, harmful strains like Clostridium difficile (C. diff) can grow unchecked, causing severe diarrhea and colitis.
4. Weakened Immune Function
Since much of your immune system resides in your gut, a disrupted microbiome can weaken your body’s defense against infections.
5. Long-Term Imbalance
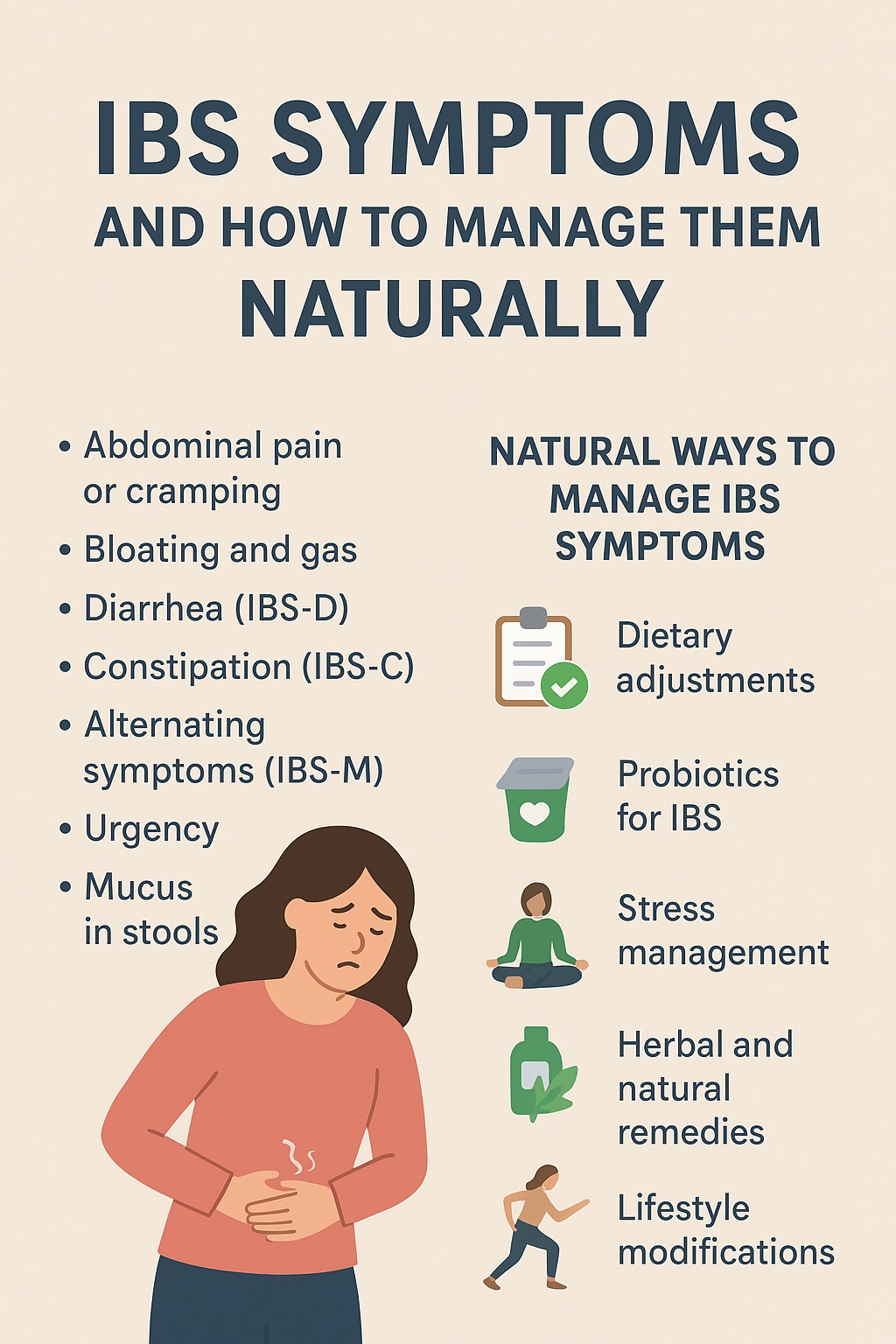
Repeated or prolonged antibiotic use may cause persistent gut issues such as food intolerances, recurring digestive discomfort, or even chronic conditions like irritable bowel syndrome (IBS).
Common Symptoms of Antibiotic-Related Gut Issues
If your gut health has been affected by antibiotics, you may notice:
- Diarrhea or loose stools
- Bloating and gas
- Stomach cramps
- Loss of appetite
- Fatigue or brain fog
- Food sensitivities developing after treatment
These symptoms may last for a few days or weeks, depending on the duration of antibiotic use and your overall gut resilience.
The Role of Probiotics After Antibiotics
One of the best ways to support digestive recovery is to replenish the gut microbiome with probiotics after antibiotics.
What Are Probiotics?
Probiotics are live microorganisms—often called “good bacteria”—that help restore gut balance.
Benefits of Probiotics Post-Antibiotics
- Repopulate the gut with beneficial bacteria
- Reduce antibiotic-associated diarrhea
- Strengthen the gut barrier and prevent harmful bacterial overgrowth
- Support immune function
- Enhance nutrient absorption
Best Sources of Probiotics
- Yogurt with live cultures
- Kefir (fermented milk drink)
- Sauerkraut and kimchi
- Miso and tempeh
- Probiotic supplements (with strains like Lactobacillus and Bifidobacterium)
Practical Steps for Digestive Recovery After Antibiotics
1. Take Probiotics Wisely
Start probiotics during antibiotic treatment, but take them a few hours apart from antibiotics to avoid reducing their effectiveness. Continue for at least 2–4 weeks after finishing the course.
2. Eat Prebiotic-Rich Foods
Prebiotics are fibers that feed beneficial bacteria. Foods like garlic, onions, bananas, asparagus, and oats help good microbes thrive.
3. Stay Hydrated
Antibiotics can cause diarrhea, leading to dehydration. Drinking enough water supports digestion and helps flush out toxins.
4. Focus on a Gut-Healing Diet
After antibiotics, eat foods that are easy on digestion and nourishing for the gut:
- Bone broth (rich in amino acids that repair gut lining)
- Fermented foods (natural probiotics)
- Fresh fruits and vegetables (fiber and nutrients)
- Whole grains and legumes (gradually, if tolerated)
5. Limit Processed and Irritating Foods
Avoid processed foods, excess sugar, alcohol, and artificial additives, as these can slow digestive recovery and feed harmful bacteria.
6. Get Enough Sleep
Rest is essential for immune repair and gut balance. Aim for 7–9 hours of quality sleep per night.
7. Manage Stress
Chronic stress impacts the gut-brain axis and can slow digestive recovery. Practices like meditation, yoga, and deep breathing help restore balance.
Long-Term Gut Health Tips
Even after you’ve recovered from antibiotics, maintaining strong gut health is essential:
- Eat a diverse, whole-food diet
- Include both probiotics and prebiotics regularly
- Exercise moderately for better gut motility
- Minimize unnecessary antibiotic use (always consult your doctor before taking them)
- Avoid smoking and limit alcohol consumption
When to Seek Medical Advice
Sometimes digestive issues after antibiotics may signal a more serious condition. Seek medical help if you experience:
- Severe or persistent diarrhea
- Signs of dehydration (dizziness, dark urine)
- Blood in stool
- Intense abdominal pain
- Symptoms lasting more than two weeks